What Causes Complications in Diabetic Wounds And Ulcers
In the United States around 30 million people have diabetes and many of them have diabetic wounds and foot ulcers. These wounds are slow to heal, prone to infection, require expert management and adversely affect a person’s overall health.
In order to stop diabetic wounds from getting worse, you may need proper wound care, which involves careful monitoring of the wound as well as the daily application of fresh dressings.
What Are Diabetic Wounds?
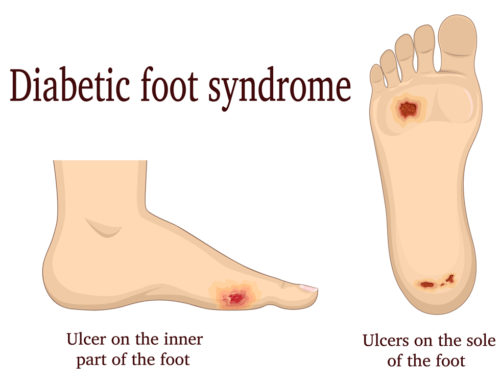
Diabetic wounds are wounds that are slow to heal in people with diabetes. This can increase the risk of infections and other complications and reduce quality of life. Foot ulcers are common in people with diabetes.

What Might Cause Diabetic Wounds?
We can’t avoid injuries in life, and sometimes even surgery, but for people with diabetes these things are doubly dangerous. High levels of blood sugar can cause diabetes, which impairs the production of insulin. And any disruption of insulin makes it more difficult for the body to manage blood glucose levels. This, in turn, slows and complicates the healing of diabetic wounds.
Also, when blood glucose remains high, it impairs the function of white blood cells. These cells are crucial for a healthy immune system. People with weak immune systems find it much harder to fight off infections and close wounds.
Poor blood circulation often accompanies diabetes, making it more difficult for the body to deliver nutrients to wounds. As a result, diabetic wounds require a lot of attention, frequent bandaging, and in some case may never heal properly.
Wound Complications
Diabetic wounds can become life-threatening if serious complications occur. It’s best to act early and prevent wounds developing to reduce the risk of wound healing complications. If you have diabetes of any kind and develop a wound or foot ulcer, be sure to seek medical advice.
Complications occur when a diabetic wound becomes infected, and the infection spreads to other parts of the body. This can result in a loss of blood supply, leading to infection and tissue destruction. Osteomyelitis is when an untreated wound infection spreads to muscle and bone.
Diabetes sufferers with persistent wounds may develop gangrene. Gangrenous tissue needs to be removed surgically without delay to avoid an amputation. Foot ulcers are common in diabetes patients, are painful, and can also lead to foot amputation.
A very severe complication is sepsis, which occurs when an infection spreads into the bloodstream, and can be life-threatening. Other diabetic wound complications include heart disease, kidney disease, and eye problems.
The information above is for educational purpose only. Do seek medical care if you have diabetes-related wounds and ulcers.
Don’t delay securing the kind of wound care you or your family member may need. Fairview Rehab & Nursing Home in Queens NY has highly experienced and skilled staff for effective treatment and management of diabetic wounds. We accept most major forms of insurance including Medicare, Medicaid, and MLTC, as well as private HMO, PPO, and EPO plans. Feel free to contact us to ask any questions you may have about the wound care we provide.
This article contains informational and educational materials and does not replace health or medical advice. For questions or concerns regarding your medical condition or health objectives, speak to a qualified physician or healthcare provider.





Leave A Comment